Abstract
Importance: Clinical evidence suggests that the time of day of treatment can affect outcomes in many different diseases, but this information is dispersed, imprecise, and heterogeneous. Consequently, practice guidelines and clinical care recommendations seldom specify intervention time.
Objective: To understand the sources of variability and summarize clinical findings on the time of day effects of medicine.
Data Sources: A systematic search of Pubmed, Google Scholar, and ClinicalTrials.gov for “chronotherapy” OR “time of administration”.
Study Selection: Any clinical study since 2000, randomized or observational, that compared the effects of treatment at different times of day. We included pharmacologic or surgical interventions having at least one continuous outcome.
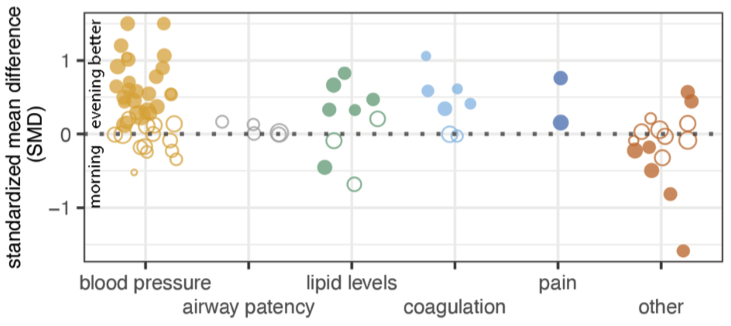
Data Extraction and Synthesis: For selected studies, we extracted the mean and variance of each time-of-day treatment group. From these, we computed the standardized mean difference (SMD) as the measure of timing effect. Where a study reported multiple outcomes, we selected a single outcome based on a defined order of priority.
Main Outcomes and Measures: We estimated overall pooled effect size and heterogeneity by a random effects model, followed by outlier detection and subgroup analyses to evaluate how study factors, including drug, design, outcome, and source, associate with timing effect.
Results: 78 studies met the inclusion criteria, comprising 48 distinct interventions over many therapeutic areas. We found an overall effect of time on clinical outcomes but with substantial heterogeneity between studies. Predicted effects range from none to large depending on the study context. Study size, registration status, and source are associated with the magnitude of effect. Larger trials and those that were pre-registered have markedly smaller effects, suggesting that the published record overstates the effects of the timing of medicine on clinical outcomes. In particular, the notion that antihypertensives are more effective if taken at bedtime draws disproportionately from one source in the field, which consistently detects larger effects than the community average. Lastly, among the most highly studied drug timing relationships, aspirin’s anti-clotting effect stands out, consistently favoring evening over morning dosing.
Conclusions and Relevance: While accounts of drug timing effects have focused on yes/no, appreciating the range of probable effects may help clarify where ‘circadian medicine’ meets the threshold for clinical benefit.
Where applicable, full text and supplement provided for fair use.